HAEMOPHILUS
BORDETELLA
BRUCELLA
PASTEURELLA
LEGIONELLA
HAEMOPHILUS
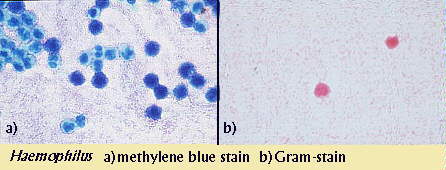
The Haemophilus genus represents a large group of Gram-negative rods
that like to grow on blood agar. The blood provides two factors which many
Haemophilus species require for growth: X factor and V factor. Sometimes
Haemophilus is cultured using something called the "Staph streak"
technique. In this procedure, both Staphylococcus and Haemophilus
organisms are grown together on blood agar. Haemophilus colonies will
usually form small colonies called "satellites" around Staphylococccus
colonies because Staph can provide the necessary factors required for
optimium Haemophilus growth. Morphologically, Haemophilus bacteria
usually appear as tiny coccobacilli under the microscope, but they are included
with the Pleomorphic bacteria because of the many shapes they assume. A
methylene blue stain of a smear can also help with identification.
Haemophilus species are classified by their capsular properties into six
different serological groups, (a-f). Species which possess a type b capsule are
clinically significant because of their virulent properties.
H. influenzae
Infection by H. influenzae is common in children and its name may lead
you to conclude that it is the causative agent of the flu. Actually, this
bacterium causes a secondary respiratory infection that usually inflicts those
who already have the flu. This species may exist with or without a pathogenic
polysaccharide capsule. Although both strains occur as normal flora of the nose
and pharynx, they can confer severe illness in patients that are
immunosuppressed or that have pre-existing respiratory ailments. Strains that
lack the capsule usually cause mild localized infections (otitis media,
sinusitis), as opposed to the type b encapsulated strain of H. influenzae
that can cause several serious infections. Most of these infections occur in
unvaccinated children less than five years of age because they have not yet
formed antibodies against the bacterium. H. influenzae infection can lead
to a variety of diseases:
- Meningitis- H. influenzae is the most common cause of
bacterial meningitis in children between the ages of five months and five
years. The initial respiratory infection can spread to the blood stream and
eventually the central nervous system. A stiff neck, lethargy, and the absence
of the sucking reflex are common symptoms in infected babies. A vaccine is
available, but is not always effective in very young children. Adult
meningitis is much less common and usually only occurs in those predisposed to
illness.
- Epiglottitis- H. influenzae is the number one cause of this
potentially fatal disease, which may cause airway obstruction in children
between the ages of 2 and 4.
- Haemophilus infection has also been associated with chronic
bronchitis, pneumonia, bacteremia, conjuctivitis, and a host of other
illnesses.
For serious infections, third generation cephalosporins are
the drug of choice. Resistance may develop when ampicillin is used in treatment.
OTHER SPECIES
H. aegyptiusThis bacterium is biochemically identical to H.
influenzae. It is known to cause pinkeye (conjuctivitis) and is spread very
easily, especially among children.
H. ducreyiChancroid, a sexually transmitted disease
characterized by painful genital ulcers, is associated with this bacterium.
H. ducreyi does not require the V factor for growth nor does it ferment
glucose.
BORDETELLA
Bordetella organisms are small, Gram-negative coccobacilli which are
strict aerobes. The three species of this genus vary in motility and certain
biochemical characteristics. The most important species in this genus is B.
pertussis, the organism which causes whooping cough. This highly
contagious bacterium makes its way into the respiratory tract via inhalation and
subsequently binds to and destroys the ciliated epithelial cells of the trachea
and bronchi. It does this through the use of several toxins:
- Pertussis toxin- an exotoxin which enters target cells and
activates their production of cAMP, a molecule that acts as a second messenger
in cell protein synthesis regulation
- Tracheal cytotoxin- causes ciliated epithelial cell destruction
- Hemoagglutinin- a cell surface protein which helps the bacterium
bind to the host cell surface
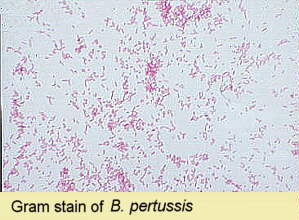 Under the
microscope, Bordetella are often bipolar stained and appear singly or in
pairs. The best method for isolation of Bordetella is on Bordet-Gengou
agar or Regan-Lowe medium. Under the
microscope, Bordetella are often bipolar stained and appear singly or in
pairs. The best method for isolation of Bordetella is on Bordet-Gengou
agar or Regan-Lowe medium.
There are about 5000 cases of whooping cough per year in the United States,
usually afflicting children less than a year old. A vaccine has reduced the
incidence of this disease one hundred fold since its introduction! Despite this
extraordinary rate of eradication, controversy exists regarding the safety of
the vaccine. Antimicrobial therapy for whooping cough usually consists of
erythromycin.
Two other species of Bordetella are also of clinical importance. B.
parapertussis is a respiratory pathogen that can cause mild pharyngitis.
This bacterium is similar to B. pertussis but lacks some of the toxins
which make its sibling so nasty. Biochemical testing can easily differentiate
the two species. Bordetella bronchiseptica is usually a cause of
pneumonia, otitis media, and other respiratory infections in animals. It is
seldom known to be a human pathogen. Its motility makes it easy to distinguish
from the other two organisms in this genus.
| DIFFERENTIATION OF BORDETELLA SPECIES |
|
Growth on
Blood Free Peptone |
Urease |
Nitrate
Reduction |
Motility |
Citrate |
| B. pertussis |
- |
- |
- |
- |
- |
| B. parapertussis |
+ |
+ |
- |
- |
+ |
| B. bronchiseptica |
+ |
+ |
+ |
+ |
+ |
BRUCELLA
Brucella is another strictly aerobic, Gram-negative coccobacillus
which causes Brucellosis. This organism is sometimes carried by animals and only
causes incidental infections in humans. The four species of this genus that can
infect humans are named for the animal which they are most commonly found: B.
abortus (cattle), B. suis (swine), B. melitensis (goats),
B. canis (dogs). The cattle and dairy industries seem to be the primary
source of infection in the United States. Brucella can enter the body via
the skin, respiratory tract, or digestive tract. Once there, this intracellular
organism can enter the blood and the lymphatics where it multiplies inside
phagocytes and eventually cause bacteremia (bacterial blood infiltration).
Symptoms vary from patient to patient but can include high fever, chills, and
sweating. Afflicted individuals are usually treated with streptomycin or
erythromycin.

PASTEURELLA
Organisms of the genus Pasteurella are Gram-negative, non-motile,
facultatively anaerobic coccobacilli. Unlike most of the pleomorphic organisms
we have spoken of, Pasteurella is not an intracellular parasite. P.
multocida is the species which most commonly infects humans. Although most
members infect animals, humans can acquire the organism from dog or cat bites.
Patients tend to exhibit swelling, cellulitis, and some bloody drainage at the
wound site. Infection may also move to nearby joints where it can cause swelling
and arthritis (not to mention a lot of pain). Fortunately, P. multocida
is susceptble to penicillin, tetracycline, and chloramphenicol. For
identification, this organism can be cultured on chocolate agar and can produce
a really foul odor.

LABORATORY INDICATIONS:
- Oxidase +
- Non-motile
- Catalase +
- Non-hemolytic (some are beta-hemolytic)
- Indole +
- Ornithine decarboxylase +
LEGIONELLA
The first discovery of bacteria from genus Legionella came in 1976
when an outbreak of pneumonia at an American Legion convention led to 29 deaths.
The causative agent, what would come to be known as Legionella
pneumophila, was isolated and given its own genus. The organisms classified
in this genus are Gram-negative bacteria that are considered intracellular
parasites. They grow well on buffered charcoal yeast extract agar, but it takes
about five days to get sufficient growth. When grown on this medium, Legionella
colonies appear off-white in color and circular in shape. Laboratory
identification can also include microscopic examination in conjunction with a
direct flourescent antibody (DFA) test. Since the initial discovery many species
have been added to the Legionella genus, but only two are within the
scope of our discussion: L. pneumophila and L. micdadei.
LABORATORY INDICATIONS:
- Motile
- Urease -
- Catalase +
- Nitrate -
- Gelatinase +
L. pneumophilaL. pneumophila is the bacterium associated
with Legionnaires' disease and Pontiac fever. Respiratory transmission of this
organism can lead to infection, which is usually characterized by a gradual
onset of flu-like symptoms. Patients may experience fever, chills, and a dry
cough as part of the early symptoms. Patients can develop severe pneumonia which
is not responsive to penicillins or aminoglycosides. Legionnaires' disease also
has the potential to spread into other organ-systems of the body such as the
gastrointestinal tract and the central nervous system. Accordingly, patients
with advanced infections may experience diarrhea, nausea, disorientation, and
confusion. The 1200 or so cases of Legionnaires' disease per year in the United
States usually involve middle-aged or immunosuppressed individuals. Pontiac
fever is also caused by L. pneumophila but does not produce the severity
of the symptoms found in Legionnaires' disease. The flu-like symptoms are still
seen in Pontiac fever patients but pneumonia does not develop and infection does
not spread beyond the lungs. Most L. pneomophila infections are easily
treated with erythromycin.
LABORATORY INDICATIONS:
- Beta-lactamase +
- Hippurate hydrolysis +
L. micdadeiL. micdadei is the second most commonly
isolated member of Legionella. This bacterium can cause the same flu-like
symptoms and pneomonia which characterize an L. pneumophila infection.
Unlike its relative, L. micdadei is sensitive to the penicillins because
it does not produce beta-lactamase.
LABORATORY INDICATIONS:
- Beta-lactamase -
- Hippurate hydrolysis -
- Acid fast
|
