THE PHARMACOLOGY OF ADRENERGIC RECEPTORS
This study guide is designed to facilitate the understanding
of sympathomimetics and sympatholytics and the adrenergic receptors at which these drugs interact to produce their therapeutic
as well as toxic effects. A web site containing this material is also available at:
http://www.mc.uky.edu/pharmacology/mtp_research.asp
Internet Sources of Drug Information
The use of the Internet as a source of drug information has
expanded significantly. The following are but a few sites which have drug information.
http://www.cp.gsm.com Clinical Pharmacology 2000 provides comprehensive monographs
on drugs currently available for clinical use.
http://www.merck.com/pubs/ This site links to a variety of publications for health care
professionals.
http://www.phrma.org/searchcures/newmeds/ Provides information on drugs which are in clinical trials
as well as those recently approved for clinical use.
http://www.rxlist.com Provides information for both the professional as well as the
consumer.
Learning Objectives, Lecture I
- Integrate pharmacodynamic principles to aid in the understanding
of adrenergic receptors and the actions of drugs on these receptors.
- Understand the criteria upon which alpha and beta receptors
are defined.
- Understand the second messenger systems utilized by alpha
and beta receptors and how activation of these receptors leads to a change in physiologic function.
- Understand the effects of alpha and beta receptor activation
on the heart and blood vessels.
- Understand the effects of isoproterenol, epinephrine and
norepinephrine on the cardiovascular system.
- Understand the rationale for the use of epinephrine in dental
practice.
Key drugs
Isoproterenol - Isuprel
Epinephrine - Adrenalin
Norepinephrine-
Levophed
The adrenergic receptors which subserve the
responses of the sympathetic nervous system have been divided into two discrete subtypes: alpha adrenergic receptors (alpha
receptors) and beta adrenergic receptors (beta receptors). The classification of these receptors, and indeed receptors in
general, is based on the interaction of agonists and antagonists with the receptors.
Beta Receptors
Beta receptors have been further subdivided into beta1
and beta2 receptors. It should be pointed out that beta3 and beta4 receptors have recently
been isolated, cloned and characterized. The beta3 receptor may be involved in regulating the metabolism of fatty
acids. This receptor could be the site of antiobesity drugs in the future. The functions of the beta4 receptor
remains to be discovered. For the purposes of this material we will focus on the beta1 and beta2 receptors
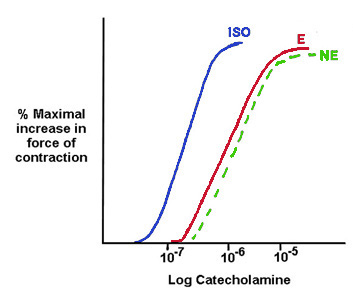
only. The classification of beta receptors is based on the the interaction of a series of drugs with these receptors. The
ability of epinephrine, norepinephrine and isoproterenol to increase the force of myocardial contraction was examined and
the following dose-response curves were obtained. Equilibrium dissociation constants for these ligands were ISO, 80 nm, E,
800 nM, and NE, 1000 nM. Thus, the rank order of affinities for the beta receptor in the heart is ISO>E>NE. A beta receptor
with these characteristics is referred to as a beta1 receptor. The equilibrium dissociation constant is often used
as a "finger print" to identify a receptor. Regardless of its location, the receptor will interact in the same manner with
ligands and have the same dissociation constants for agonists and antagonists.
|
|
Conversely, if the ability of the same compounds to produce
bronchodilation was examined, a different set of dose response curves and equilibrium dissociation constants were obtained.
The dissociation constants were ISO, 80 nm, E, 800 nM, and NE, 10,000 nM Clearly then the receptor in the lung is different
from that in the heart and is referred to as a beta2 receptor. It should be apparent how dissociat-ion constants
can be used to define and discover new receptors.
Beta Receptor Systems
Most tissues express multiple receptors. However, the dominant
beta receptor in the normal heart is the beta1 receptor while the beta2 receptor is the dominant regulatory
receptor in vascular and nonvascular smooth muscle.
| Tissue |
Receptor Subtype |
| Heart |
beta1 |
| Adipose tissue |
beta1beta3? |
| Vascular Smooth Muscle |
beta2 |
| Airway Smooth Muscle |
beta2 |
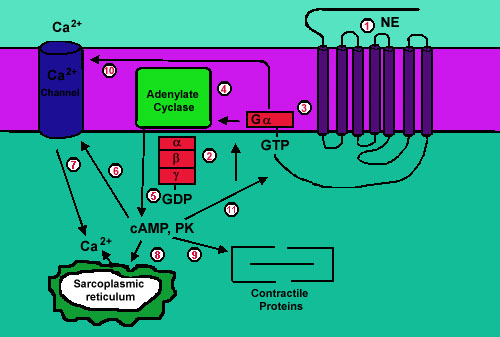
Mechanism of Beta Receptor Activation in Cardiac Muscle
1. Agonist binds to the myocardial beta1-receptor.
The receptor is a typical G-protein coupled receptor with 7 membrane spanning regions.
2. G-protein complexed with
GDP.
3. The receptor promotes exchange of GTP for GDP and release
of Gα complexed with GTP.
4. Gα activates adenylate cyclase.
5. ntracellular cAMP increases and activates cAMP dependent
protein kinase (PKA).
6-10 PKA phosphorylates cellular effectors leading to a positive
inotropic response.
11. Prolonged stimulation can lead to receptor down-regulation
via PKA and other protein kinases which induced phosphorylation of the receptor. The other protein kinases which are involved
in phosphorylation of the receptor are referred to as G-protein coupled receptor kinases or GRKs. These phosphorylation steps
lead to internalization of the receptor.
|
|
Effect of Beta Receptor Activation on the Heart: Activation
of the beta1 receptor leads to increases in contractile force and heart rate. Excess stimulation by catecholamines
can induce significant increases in heart rate and arrhythmias. Arrhythmias are a major concern with drugs such as E, NE and
ISO that can activate the beta1 receptor.
Effect of Beta Receptor Activation on Smooth Muscle: The
beta2 receptor associated with smooth muscle also utilizes the cAMP signaling system. However, the results of receptor
activation are different. Stimulation of the beta2 receptor leads to smooth muscle relaxation. This is because
in the pathways leading to activation of myofibrillar proteins and contraction are different in smooth muscle when compared
to cardiac muscle. Therefore, steps 1-5 in the diagram would be the same. However, the cellular proteins phosphorylated by
PKA are different in smooth muscle when compared to cardiac muscle.
ALPHA RECEPTORS SYSTEMS:
If the ability of isoproterenol, epinephrine and norepinephrine
to produce constriction of vascular smooth muscle is studied, the following dose-response curves and equilibrium dissociation
constants were obtain E, 5 uM, NE, 6, uM and ISO, 1000 uM. You should begin to understand the reasons why the receptor causing
vasoconst-riction MUST be different from that causing cardiac contracti-on or broncodil-ation.
The receptor mediating the vasconstrictor actions
of catecholamines is referred to as an alpha receptor. The concentration of isoproterenol necessary to activate alpha receptors
is so large that isoproterenol can be thought of as a pure beta receptor agonist.
Alpha receptors have been further subdivided into alpha1
and alpha2 receptors. Epinephrine and norepinephrine are equipotent at both alpha1 and alpha2
receptors. Three subtypes of the alpha1-receptor, the alpha1A, the alpha1B, and the alpha1D,
and 3 subtypes of the alpha2-receptor, the alpha2A, the alpha2B, and the alpha2C
have been isolated, cloned and characterized. However, we will refer to only the alpha1 and alpha2 receptors.
Postsynaptic
Alpha1 And Alpha2 Receptors:
Alpha1 and alpha2 receptors exist postsynaptically.
Activation of these receptors in vascular smooth muscle leads to Ca2+ influx and release of Ca2+ from
intracellular stores. The increased intracellular Ca2+ activates vasoconstriction.
-
Agonist binds to the vascular smooth muscle
alpha1-receptor. The receptor is a typical G-protein coupled receptor with 7 membrane spanning regions.
-
G-protein complexed with GDP.
-
The receptor promotes exchange of GTP for GDP
and release of Gα complexed with GTP.
-
The G-protein activates phospholipase C leading
to an increase of the intracellular second messengers, inositol trisphosphate (IP3) and diacylglycerol (DAG).
-
IP3 binds to specific sites on the SR and stimulates
the release of intracellular Ca2+.
-
Ca2+ influx is activated.
-
Like the beta-receptors, alpha receptors can
also be desensitized and down regulated via phosphorylation of the receptor. However, the alpha receptors, both alpha1
and alpha2 are much more resistant to desensitization and down regulation than are the beta receptors.
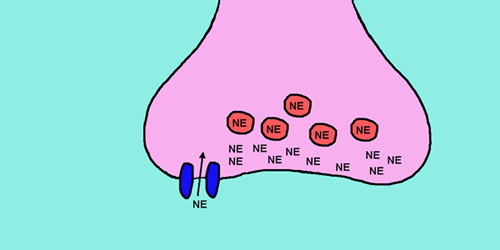
Presynaptic Alpha2 Receptors
Alpha2 receptors also exist presynaptically associated
with nerve terminals. Activation of these receptors inhibits the release of norepinephrine. The mechanism for this
regulatory activity may be that prejunctional alpha2 receptors activate a G-protein gated K+ channel
leading to membrane hyperpolarization.
Norepinephrine acts at presynaptic alpha2
receptors to inhibit its own release.
Effect of Catecholamines on Vascular Smooth
Muscle:
Associated with vascular smooth muscle are a large number
of alpha1 receptors relative to beta2 receptors. However, epinephrine has a higher affinity for the
beta2 receptors when compared to the alpha1 receptors. Therefore, the effect of epinephrine is dependent
on which type of receptor is occupied. Recall that receptor occupancy is dependent on the concentration of a drug and its
equilibrium dissociation constant. At low doses, epinephrine can selectively stimulate beta2 receptors, thus producing
muscle relaxation and a decrease in peripheral resistance. At high doses, epinephrine produces contraction of vascular smooth
muscle and an associated increase in peripheral resistance.
Effect of Catecholamines on Vascular Smooth Muscle: (Continued)
Norepinephrine has little affinity for beta2 receptors.
Therefore, it will stimulate only alpha1 receptors, producing an increase in peripheral vascular resistance. In
contrast, isoproterenol will only produce vasodilation due to activation of the beta2 receptors.
Effects On The Cardiovascular System
Recall that:Blood pressure = Cardiac output X total peripheral
vascular resistance (TPR)Cardiac output = Stroke volume X heart rate
Therefore: Blood pressure = (stroke volume X heart rate)
X Total peripheral vascular resistance
For the drugs listed below, indicate how the drugs would
affect (increase, decrease, no changes) the indicated hemodynamic parameters. It is important, both from a basic science as
well as a clinical perspective, that you understand the actions of these agents on the cardiovascular system.
Be sure to make an attempt at answering the question BEFORE
you click on the answer.
Applications to Therapeutics
Oral dosing of norepinephrine, epinephrine and isoproterenol
is not possible due to rapid metabolism of the catechol nucleus in gastrointestinal mucosa and liver. Therefore, these agents
are given I.V., I.M., topically and in aerosol sprays. There is very limited clincial use of norepinephrine. Epinephrine is
often used in combination local anesthetic agents to prolong the duration of anesthetic action. This is accomplished because
epinephrine can induce vasoconstriction thus limiting the diffusion of the local anesthetic from the site of injection. This
serves to reduce the toxicity of the local anesthetic by limiting its systemic absorption. Lidocaine in toxic doses can produce
cardiac arrthythmias and convulsions. Epinephrine can also be topically applied in surgical procedures to induce vasoconstriction
and thus reduce blood loss. Epinephrine is used in the treatment of shock and in emergency situations related to bronchial
asthma. A major concern with using pressors is the effect on systemic arterial pressure. Clinical studies have shown (for
example see Table 6.5 in Yagiela et al, p. 109) that epinephrine blood levels increase following its intraoral administration.
The risk of this increase is dependent on characteristics of the patient. For example, hypertensive patients or those with
other cardiovascular disease or patients taking other drugs that affect sympathetic nervous system function are at higher
risk than patients without these conditions. Systemically absorbed epinephrine could also increase heart rate and exacerbate
cardiac rhythm disturbances or myocardial ischemia.
Learning Objectives Lecture II
- Understand the potential sites of action for sympathomimetics
and sympatholytics.
- Understand the pharmacologic actions and therapeutic effects
of dopamine.
- Understand how the pharmacodynamic actions of dopamine illustrate
the properties of a drug that interacts with multiple receptors.
- Know that there are beta2 agonists, their mechanisms
of action and therapeutic uses.
- Know the mechanism of action and cardiovascular effects
of amphetamine and cocaine.
- Know the effects and therapeutic uses of drugs that can
activate the alpha1 adrenergic receptors.
Key Drugs*
Amphetamine-Adderall
Albuterol - Ventolin - 13th
leading prescription drug in the US in 2003- source- rxlist.com
Cocaine
Dopamine - Intropin
Methylphenidate
- Ritalin - 102nd leading prescription drug in the US in 2003- source- rxlist.com
Phenylephrine - Neosynephrine
* A more complete list of sympathomimetics and their trade
names can be found on p. 110-111 of the Yagiela text.
Sympathomimetics: synthetic analogs of naturally
occurring catecholamines that mimic the actions of the endogenous neurotransmitters. These agents can be divided into direct
and indirect acting sympathomimetics.
Sympatholytics: synthetic analogs which bind to beta or alpha
receptors or act through other mechanisms to block the actions of endogenous neurotransmitters or other sympathomimetics.
In addition to interacting with receptors, adrenergic agonists
and antagonists can interact at sites on the nerve terminal to produce sympathomimetic or sympatholytic effects. These potential
sites are indicated by the numbers. A clear majority of drugs are direct acting agonists or antagonists. A small number of
drugs work through the other listed mechanisms.
- Direct acting agonists or antagonists can act at postsynaptic
receptors.
- Indirect acting agonists release neurotransmitters from
presynaptic nerve terminals to produce a sympathomimetic effect.
- Drugs such as Guanethidine can inhibit the Ca2+-dependent
release of norepinephrine, thus having a sympatholytic effect.
- Drugs such as Reserpine cause the destruction of storage
granules, and as a result, depletion of the synaptic terminal of norepinephrine which is also a sympatholytic action.
- Inhibition of the membrane uptake of catecholamines by drugs
such as cocaine and tricyclic antidepressants produce a sympathomimetic effect.
- Inhibition of monoamine oxidase by drugs such as Tranylcypromine.
SYMPATHOMIMETICS ACTING AT BETA RECEPTOR SYSTEMS
EXAMPLES:
Dopamine
Beta2 agonists
DOPAMINE-An illustration of the actions of a drug that activates
multiple receptorsDopamine has a complex pharmacology. It can activate at least 4 different receptors: the beta1,
dopamine1 (DA1), alpha1 and alpha2. DA1 receptors exist in the renal
vascular bed. Activation of these receptors produces a decrease in renal vascular resistance and an increase in renal blood
flow. Activation of the beta1 receptor increases the force of myocardial contraction. Dopamine has a very unusual
action on the heart in that it selectively increases the force of myocardial contraction without a significant effect on heart
rate. However, high doses of dopamine, like all catecholamines which activate the beta1 system, can induce rhythm
disturbances. The beneficial effects of dopamine are due to stimulated DA1 and beta1 - receptors. Activation
of the alpha1 receptor will produce increases in vascular resistance which is counterproductive to the effects
on the heart and kidney. The increase in peripheral resistance would increase the pressure the heart has to work against and
hence act to decrease cardiac output.

Uses of Dopamine
Dopamine can be used to treat congestive heart failure
and cardiogenic shock.
In congestive heart failure, the failing heart is not able
to eject blood as efficiently as the normal heart. As a result there is a decrease in cardiac output which triggers a host
of compensatory actions. These include fluid retention, vasoconstriction, an increase in peripheral vascular resistance, and
an increase in the levels of circulating catecholamines and tissue hypoxia. Dopamine is particularly effective in these situations
because of its actions on the heart and renal vasculature. The actions on the heart will increase cardiac output while the
effects on renal blood flow will produce diuresis and loss of excess fluid.
Pharmacokinetics of Dopamine
Dopamine is similar to epinephrine and norepinephrine as
it has a short plasma half life and can only be used I.V.
SELECTIVE BETA2 AGONISTS
These agents have a higher affinity (lower equilibrium dissociation
constant) for beta2 receptors when compared to beta1. Therefore, they selectively activate beta2
receptors when compared to beta1. The cellular action of these drugs is mediated by cAMP.
Uses
1) Airways dysfunction; bronchial asthma, chronic bronchitis,
emphysema
In airways dysfunction, beta2 selective agonists
relax airways thus decreasing airways resistance.
2) Premature labor
In premature labor, the beta2 selective agonists
relax uterine smooth muscle. Drugs that relax uterine smooth muscle are referred to as tocolytic agents.
ALPHA1 AGONISTS
Direct Acting Agents
These are synthetic agents that directly activate the alpha1
-adrenergic receptor. These structural modifications of the parent catecholamine nucleus result in drugs that are orally active
and have longer plasma half-lives. However, these same modifications result in lower affinity for the receptor than do the
endogenous agonists (epinephrine or norepinephrine). There are 2 structural classes of alpha1 agonists:
| Phenylethylamines |
Imidazolines |
| Phenylephrine |
Oxymetazoline |
| Methoxamine |
Naphazoline |
| Metaraminol |
Tetrahydrozoline |
| Ephedrine |
|
_____________________________________________________________________________
_____________________________________________________________________________
Indirect Acting Agents
Indirect Acting Agents that activate Alpha Receptors
These agents require the presence of endogenous catecholamines
to produce their effects. They have little activity if catecholamines are depleted.
Cocaine: Blocks reuptake of NE into nerve endings.
Amphetamine: Promotes the release of NE from nerve endings. The NE
is not released from vesicles but from the cytoplasmic stores of NE. This is also referred to as the mobile pool. There is
only a limited amount of NE in this mobile pool. Therefore, tachyphylaxis to the sympathomimetic actions of amphetamine can
develop. Amphetamine can also block the reuptake of norepinephrine.
Amphetamine-like congeners
1.
Methylphenidate
2. Pemoline
3. Methamphetamine
A major site action of cocaine, amphetamine
and amphetamine-like agents is in the CNS. These drugs produce a feeling of well being and euphoria. There is very limited
therapeutic use of cocaine and amphetamine. Analogs of amphetamine are used to treat hyperactivity in children and act as
appetite suppressants. In addition to its effects on the uptake of neurotransmitters, cocaine also has local anesthetic properties.
It is used for local anesthesia and vasoconstriction in surgical procedures involving oral, laryngeal or nasal cavities.
Applications to Therapeutics
- Dental-The use of epinephrine and other pressor agents in
dental practice has previously been discussed.
- Hypotension-to increase blood pressure during a surgical
procedure where a general anesthetic has induced hypotension
- Ophthalmic preparations-to induce mydrasis also in topical
preparations for symptomatic release of eye irritation.
- Cough and cold preparations-Induces constriction of nasal
mucosa decreases resistance to air flow.
- CNS actions - Amphetamine and congeners
a. Appetite
suppression -
b. Hyperactivity in children -
Cocaine and amphetamine-like agents could potentiate the
effects of direct acting agonists such as epinephrine. Recall that epinephrine can be absorbed systemically after intraoral
administration. Thus, the risk of hypertension and other problems associated with systemic absorption of epinephrine will
be greater in patients taking cocaine or amphetamine-like drugs. This is because the actions of epinephrine are terminated
in part by uptake into the synaptic terminal.
Learning Objectives Lecture III
- Understand how activation of α2 receptors
decreases sympathetic outflow and cause hypotension.
- Understand the pharmacologic properties and therapeutic
uses for prazosin-like drugs.
- Understand the pharmacologic properties of propranolol and
atenolol and the therapeutic uses of beta-adrenergic receptor blockers.
- Understand the special precautions needed for sympatholytic
drugs in dental practice.
Key Drugs*
Atenolol - Tenormin and various trade names - 4th
leading prescription drug in the US in 2003- source- rxlist.com
Clonidine - Minipres, various trade names
Propranolol - Inderal - various trade names
Terazosin - Hytrin
* A more complete list of sympatholytics and their trade
names can be found on p. 123 of the Yagiela text.Alpha2 Agonists As Sympatholytics
-
Clonidine
-
Methyldopa
-
Guanabenz
Actions
- These drugs stimulate alpha2 receptors in the
nucleus tractus solitarius (NTS) to decrease sympathetic outflow to the heart and blood vessels.
- The decrease in sympathetic tone results in a decrease in
peripheral vascular resistance.
- Clonidine and guanabenz are active drugs.
- Methyldopa is a prodrug which must first be converted to
α-methylnorepinephrine.
SELECTIVE ALPHA1-ANTAGONISTSPrazosin and analogs.
Prazosin was the first selective alpha1-receptor antagonist that was developed. Several analogs have since been
developed.
Effects of Prazosin and Analogs on the Cardiovascular
System:
- Relaxes arterial and venous smooth muscle as well as nonvascular
smooth muscle.
- Decreases peripheral vascular resistance and venous return.
- Decreases systemic arterial blood pressure without a significant
increase in heart rate.
- Prazosin analogs - terazosin, doxazosin, trimazosin; the
beneficial effects of these drugs are the same, but they differ in pharmacokinetic properties.
Uses
1. Hypertension
2. Benign prostatic
hypertrophy
Side Effects1. Orthostatic hypotension. Orthostatic hypotension
is a problem with prazosin as well as vasodilators that affects the tone on venous smooth muscle. This would include, organic
nitrates, hydralaizne, minixodil and the many drugs used to treat impotence. Orthostatic hypotension or postural hypotension
occurs when systemic arterial blood pressure falls by more aht 20 mmHg upon standing. In this situation, cerebral perfusion
falls and an individual may become light headed, dizzy or pass out. In changing from the supine to the standing position,
gravity tends to cause blood to pool in the lower extremities. However, several reflexes, including sympathetically mediated
venoconstriction minimize this pooling and maintain cerebral perfusion. If these reflex actions do not occur, then orthostatic
hypotension could result. By blocking the alpha1-receptors associated with venous smooth muscle, prazosin-like
drugs, blood the sympathetically mediated vasoconstriction associated with postural changes. Hence, Orthostatic hypotension
can occur.BETA ADRENERGIC RECEPTOR BLOCKERS
- These drugs are competitive antagonists of the beta adrenergic
receptors
- Beta blockers are either selective for the beta1
receptor or nonselective beta1 and beta2antagonists.
SELECTIVE AND NONSELECTIVE BETA BLOCKERS
Propranolol - The Prototype Beta Blocker:
- Blocks myocardial beta1 receptors which is a
major site of therapeutic action
- Cardiovascular effects:
a. Decreases force and rate
of myocardial contraction
b. Decreases renin secretion
c. Decreases blood pressure
- Blocks beta2 receptors, the blockade of receptors
produces unwanted side effects
Cardiovascular Uses
1. Hypertension
2. Ischemic heart disease
3. Supraventricular tachyarrhythmias
Disadvantages of Nonselective Beta Blockers
A major disadvantage of nonselective beta blockers is the
fact that they will block beta2 receptors associated with airway or vascular smooth muscle. This is a problem in
treating patients with airway dysfunction or peripheral vascular disease such as alpha1 adrengeric receptor-mediated vasoconstrictor
tone will be unoppsed by the beta2 receptors. To overcome this disadvantage, antagonists that selectively block
the beta1 receptor have been developed. However, this selectivity is only relative and in higher doses selective
antagonists will also block beta2 receptors.
Endocrine Effects
- Non-selective beta blockers are contraindicated in
diabetic patients. Selective beta1 blockers should be used with caution in patients with diabetes. This is because
catecholamines utilize the beta2 receptor to promote
glycogenolysis and mobilize glucose. This effect would
be blocked by non-selective beta blockers.
- In addition all beta blockers mask the tachycardia associated
with hypoglycemia. As a result, the diabetic patient is deprived of one of the earliest physiologic responses to hypoglycemia.
Side Effects
- Sedation, fatigue
- Exacerbation of peripheral vascular disease, airway dysfunction
Monoamine Oxidase Inhibitors
- These drugs inhibit monoamine oxidase and are used as antidepressants
in psychiatric practice.
- A side effect that is not clearly understood is that these
drugs can also produce hypotension.
- Can precipitate a hypertensive crisis.
Uses
- Hypertension
- Depression
Applications to Therapeutics-excerpted from Chapter 7, p.123
of the Yagiela text
Many of the agents discussed in this chapter are widely used
to treat hypertension, ischemic heart disease, congestive heart failure and rhythm disturbances. This has important implications
in the practice of dentistry and signals the dentist's need to pay heed to potential risks associated with these conditions.
Physical ImplicationsA consideration for patients being treated
with some sympatholytics is the patient's position during and after dental procedures. Suddenly standing upright after being
in a supine position in the dental chair is very apt to cause syncope. This is particularly true for the antihypertensive
drugs more prone to cause orthostatic hypotension (e.g., prazosn and other α1 -adrenergic receptor blocking
drugs, drugs with combined α- and β-receptor blocking activity and adrenergic neuron blocking agents). Accidents
ranging from broken teeth and restorations to fractured mandibles and worse have resulted from falls. Contemporary practice
standards require the monitoring of blood pressure in dental patients. Such monitoring is particularly important in hypertensive
patients.
Drug InteractionsBecause nonselective β-blockers block
β2-receptor mediated vasodilation, there is a risk of a hypertensive episode following administration of local
anesthetic agents that contain vasoconstrictors or the use of epinephrine-impregnated retraction cords. In this situation,
the vasoconstrictor actions of epinephrine at α1 -receptors are not opposed by the vasodilatory actions of
β2-receptors resulting in an exaggerated blood pressure response that could be deleterious in patients with
hypertension or ischemic heart disease.
Clonidine and the other selective β2-adrenergic
receptor agonists are among the drugs that cause xerostomia. This effect also occurs with reserpine and, less frequently,
with α-adrenergic receptor antagonists. The use of such drugs may result in clinical symptoms related to dry mouth, such
as difficulty in swallowing and speech. Chronic use of xerostomia-producing drugs is associated with a higher incidence of
oral candidiasis and dental caries. The use of β -adrenergic receptor blockers is likely to alter the composition of
salivary proteins. The effects of these changes have not been fully explored; however, there is a concern that they could
adversely influence oral health. The effect of drugs that alter the function of adrenergic nerve endings on salivary proteins
is also not well explored.
Patients taking MAO inhibitors must not be given drugs that
have indirect sympathomimetic activity or are inactivated by MAO. Occasionally, the dentist may find reason to use the vasoconstrictor
phenylephrine. Because it causes even a minor release of norepinephrine from adrenergic nerves and is subject to metabolism
by MAO, phenylephrine must be avoided in patients taking MAO inhibitors. Epinephrine and levonordefrin, which are most commonly
found in local anesthetic solutions, are not contraindicated, since they are direct agonists and are largely inactivated by
catechol-O-methyltransferase. Nonetheless, the avoidance of hemostatic preparations containing high concentrations of epinephrine
is recommended.
Opioids and other CNS depressants should be used cautiously
and usually at lower doses in patients who are taking MAO inhibitors. Meperidine is absolutely contraindicated. The dentist
should reinforce the physician's instructions to the patient about dietary restrictions and contraindications of several drugs
for patients taking MAO inhibitors.
For the drugs bretylium, reserpine, guanadrel and guanethidine,
a condition resembling denervation supersensitivity may be clinically significant; the intensity of the response to exogenous
amines may be increased several fold as a result. This increased sensitivity does not usually contraindicate the use of vasoconstrictors
in local anesthetic solutions; however, caution must be exercised to avoid accidental intravenous injection and giving high
amounts of a vasoconstrictor. The use of adrenergic hemostatic agents, as found in certain gingival retraction cords, is best
avoided.
The following is a list of trade names for the drugs mentioned
in this handout. It is provided for your information.
| Epinephrine |
Adrenalin Chloride |
| Phenylephrine |
Neo-synephrine |
| Isoproterenol |
Isuprel |
| Norepinephrine |
Levophed |
| Methoxamine |
Vasoxyl |
| Metaraminol |
Aramine |
| Clonidine |
Catapres |
| Methyldopa |
Aldomet |
| Guanabenz |
Wytensin |
| Oxymetazoline |
Afrin |
| Naphazoline |
Naphcon Forte Ophthalmic |
| Tetrahydrozoline |
Tyzine |
| Prazosin |
Minipress |
| Terazosin |
Hytrin |
| Doxazosin |
Cardura |
| Acebutolol |
Sectral |
| Atenolol |
Tenormin |
| Betaxolol |
Betopic, Kerlone |
| Bisoprolol |
Zebeta |
| Esmolol |
Brevibloc |
| Metoprolol |
Lopressor, Toprol XL |
| Carteolol |
Cartrol |
| Nadolol |
Corgard |
| Penbutolol |
Levatol |
| Pindolol |
Visken |
| Propanolol |
Inderal |
| Sotalol |
Betapace |
| Timolol |
Blocadren |
| Labetalol |
Trandate, Normodyne |
| Salmeterol |
Serevent |
| Albuterol |
Proventil, Ventolin |
| Bitolterol |
Tornalate |
| Isoetharine |
Bronkosol |
| Metaproterenol |
Alupent, Metaprel |
| Pirbuterol |
Maxair |
| Terbutaline |
Serevent |
| Guanethidine |
Ismelin |
| Reserpine |
----- |
